Beyond the toothache: How Clark County is responding to an oral health crisis
County leaders are bridging gaps in oral health by improving access, affordability, and workforce shortages through outreach, education, and partnerships.

Like many places in rural America, Clark County is facing a persistent oral health gap that leaves many residents struggling to access even the most basic dental care. It doesn’t help that, for years, oral health has been removed from broader healthcare discussions nationally and regionally. Finding this reality unacceptable, a coalition of local stakeholders decided to address the gaps head-on.
Since 2017, the Community Health Foundation has spearheaded the Clark County Oral Health Coalition to address what was long viewed as an overlooked health crisis. As Community Health Foundation’s Grants and Program Manager Faith Bosland explains, it’s high time for oral health to enter the mainstream conversation around healthcare.
“Dental care just gets siloed from healthcare due to the way the system is designed. There’s not a lot of concerted effort to give this coordinated attention in our community.”
According to Bosland, the lack of coordination has real consequences.
It’s common for residents to face long wait times, transportation barriers, and, increasingly, a dire shortage of oral health providers, she explains. Most dental practices in the county are small businesses with packed patient schedules, leaving little room for new patients — especially those relying on Medicaid or without insurance. Rocking Horse Community Health Center, the local Federally Qualified Health Center (FQHC), is one safety net provider, but it has struggled to keep up.
“They had to close their wait list because they hit capacity so quickly,” Bosland says.
The workforce gap is acute in Clark County, adding a layer of complexity. According to Bosland, every level of the dental profession — dentists, hygienists, and assistants — is feeling the crunch. But the shortage of dental hygienists is especially impactful. Bosland says that local practices report that not having enough hygienists can mean up to 1,500 fewer patient visits per hygienist per year.
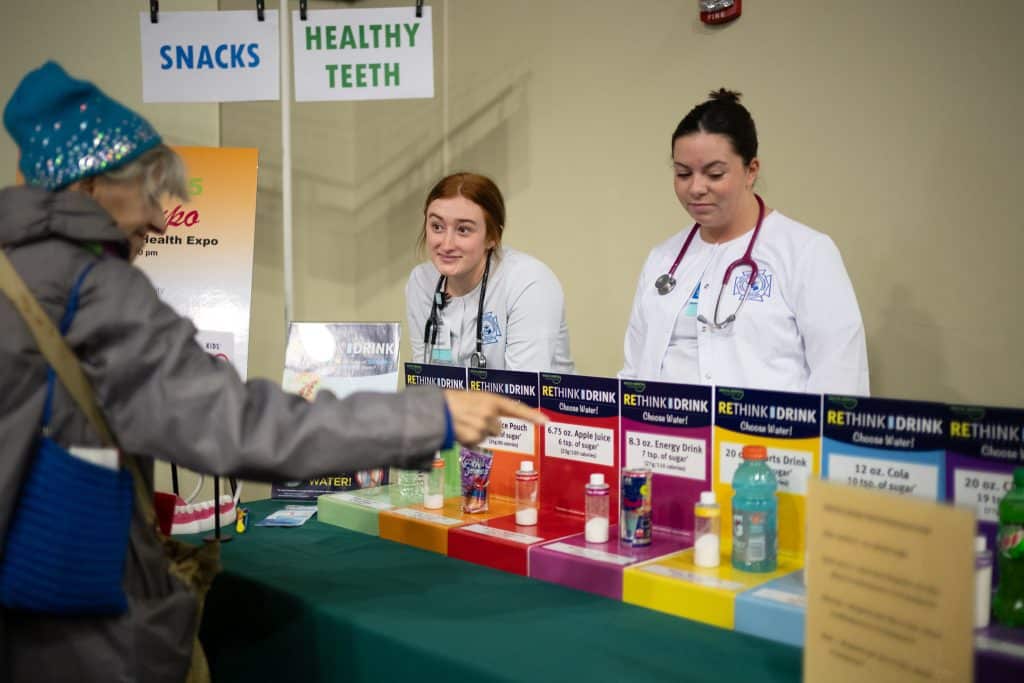
Photo by Andy Grimm.
Bosland cites the findings of a 2023 coalition survey, which further drive home this point. For example, 100% of participating practices reported serious difficulty hiring hygienists, and 67% struggled to hire dental assistants. Extrapolated, Clark County practices expect they’ll need to hire more than 75 dental assistants and about 40 hygienists over the next three years. This is an unsustainable gap given current training and recruitment trends.
In response, Clark County leaders have focused on systems-level change, bringing together diverse stakeholders, including dental providers, the health department, health clinics, schools, Head Start agencies, and representatives from business and mental health, in coordinated action.
One approach targets the workforce pipeline itself. Recognizing that too few students are entering dental careers, the coalition works to promote dental professions among high schoolers, calling attention to opportunity and community impact.
Yet, even as student interest grows, bottlenecks present hurdles. Per Bosland, the region’s dental hygiene programs have long waitlists, and most lack the capacity to meet demand. This aligns with national data. According to the trade publication Dimensions of Dental Hygiene, the US has 335 accredited dental hygiene programs with an overall capacity of 9,815 positions for students/learners annually.
The coalition also supports loan repayment incentives for hygienists and dentists who work in community health centers. This incentive helps recruit young professionals who may be saddled with student loan debt.

Another solution introduced by the coalition focuses on expanding access for under-resourced populations. In this context, mobile dental clinics travel to schools and community centers. The idea is to reduce transportation barriers and reach children who might never see a dental provider otherwise.
Community education is a mainstay as well. Bosland says that outreach includes distributing thousands of toothbrush kits to kindergarten and first-grade students each year. They work with nursing students to deliver in-school presentations and partner with teachers and nurses to integrate oral health education into the curriculum. These efforts, aimed at prevention, can instill lifelong healthy habits that can lead to favorable outcomes well into adulthood.
Recognizing the unique needs of the county’s growing immigrant population, the coalition also looks to recruit and develop a more bilingual dental workforce.
“Our dentists really would love to hire more bilingual staff,” Bosland says.
This is an important edge, as culturally informed care has been shown to improve communication and deepen trust. According to Indiana Wesleyan University, “culturally competent individuals can navigate situations with a diverse range of people while accommodating and respecting their beliefs, backgrounds, cultural traditions, and social structures.” Practically speaking, Bosland says it can reduce the length of appointments and improve the accuracy of health information delivered.
As Bosland notes, county-level oral health data remains scarce. However, partners are known to measure progress through data like clinic capacity, service numbers, and stakeholder surveys. For instance, Rocking Horse Center’s rapid waitlist growth is a clear indicator of unmet demand. It can also be interpreted as a signifier of effective outreach. One potential conclusion: more previously unreached families are connecting with care.
The coalition’s workforce survey found nearly all local practices urgently need hygienists and assistants. At the same time, educational outreach — such as the annual Health Expo and school-based hygiene programs — has reached thousands of students each year. Since launching these efforts, Bosland says more children are receiving regular cleanings, and school-based screenings have caught problems before they become more costly and acute.

Despite local successes, the coalition’s results have been tempered by persistent challenges. Workforce development is wrapped up in systemic issues. Bosland cites a limited number of seats in hygiene programs, competition from higher-paying urban markets, and physical demands that can drive early retirements as factors in the mix. Loan repayment incentives and competitive salaries help, but FQHCs have restricted flexibility compared to private practices.
Most efforts to date rely on anecdotal and programmatic data. A lack of granular, county-level oral health statistics makes long-term tracking difficult. Still, Clark County’s experience sheds light on an inconvenient truth: tackling dental health requires more than piecemeal grassroots activism. It demands cross-sector collaboration, policy advocacy, and investments in public health infrastructure.
“When we invest in programs that increase access to preventative care, we’re not just saving teeth; we’re improving overall health, reducing the burden on emergency rooms, and building a stronger, healthier community for everyone,” Bosland says.